Optimizing Medical Device Manufacturing Compliance with Workflow Automation

Key takeaways
- The medical device manufacturing industry faces stringent compliance requirements, making workflow automation essential for accuracy and efficiency.
- The U.S. and EU markets have different regulatory challenges, including FDA and MDR compliance, which automation can help navigate.
- Automation enhances efficiency and innovation by streamlining production, reducing errors, and improving documentation processes.
- Design for Automation (DFA) is a key approach in medical manufacturing, ensuring devices are designed with automation-friendly processes.
- Workflow automation improves traceability, quality control, and compliance in medical device production.
- Cflow provides a robust solution for automating medical manufacturing workflows, enhancing efficiency and regulatory adherence.
Medical device manufacturing is one of the most highly regulated industries, requiring strict compliance with safety, quality, and regulatory standards. Companies operating in this sector must navigate complex approval processes, stringent documentation requirements, and evolving regulatory landscapes. Ensuring compliance while maintaining efficiency can be a significant challenge for manufacturers.
Workflow automation is transforming the medical device manufacturing industry by streamlining operations, reducing human errors, and ensuring adherence to regulatory standards. From automating quality control checks to optimizing documentation processes, automation plays a critical role in enhancing efficiency and compliance.
This blog explores the current state of medical device manufacturing, the benefits of automation, and how companies can optimize their workflows using cutting-edge automation solutions like Cflow.
Table of Contents
Current Status of the Medical Device Manufacturing Industry
U.S. Market
The U.S. medical device manufacturing industry is one of the largest globally, driven by innovation and stringent regulatory oversight from the Food and Drug Administration (FDA). Manufacturers must comply with 21 CFR Part 820, which outlines quality system regulations (QSRs) for medical devices. Key challenges include:
- Regulatory Complexity: Ensuring compliance with FDA premarket approval (PMA) and 510(k) clearances.
- Quality Assurance: Maintaining high production standards and traceability.
- Supply Chain Disruptions: Managing raw material shortages and logistics challenges.
EU Market
The European medical device industry follows the Medical Device Regulation (MDR), which has significantly increased compliance requirements. Challenges faced by manufacturers include:
- Extended Approval Timelines: Stricter MDR regulations have led to longer product certification periods.
- Post-Market Surveillance: Increased monitoring of device performance post-launch.
- Harmonization Issues: Varying interpretations of MDR regulations across EU member states.
Challenges in Compliance in Medical Device Manufacturing
Medical device manufacturers face numerous compliance challenges due to the stringent regulations and evolving industry standards. Ensuring compliance requires meticulous documentation, rigorous quality control, and seamless traceability throughout the production cycle. Below are some of the key compliance challenges that manufacturers encounter:
1. Complex Regulatory Requirements
The medical device industry must adhere to stringent regulatory frameworks such as the FDA’s 21 CFR Part 820, the EU MDR, and the ISO 13485 quality management system. These regulations demand rigorous documentation, strict adherence to manufacturing protocols, and thorough audits. Keeping up with evolving regulations and ensuring global compliance can be overwhelming for manufacturers.
2. Extensive Documentation and Record-Keeping
Compliance requires manufacturers to maintain detailed records of every step of the production process, including design controls, risk management, testing results, and post-market surveillance. Manually managing these documents can lead to errors, missing data, and non-compliance penalties. Automated documentation workflows help streamline record-keeping and ensure accuracy.
3. Quality Control and Product Safety
Medical devices must meet high safety and performance standards, making quality control a top priority. Manufacturers need to conduct extensive testing, validation, and real-time monitoring to detect defects. Failure to meet quality benchmarks can result in recalls, regulatory action, and reputational damage.
4. Supply Chain Compliance and Traceability
The complexity of global supply chains makes it challenging to track raw materials, verify supplier compliance, and ensure end-to-end traceability. Regulations such as UDI (Unique Device Identification) require detailed tracking of device components throughout their lifecycle. Automating supply chain workflows ensures seamless traceability and compliance with reporting requirements.
5. Post-Market Surveillance and Reporting
Regulatory bodies require manufacturers to monitor device performance after market release. Adverse event reporting, customer feedback management, and real-world data collection are essential for ensuring continued compliance. Manual monitoring can be time-consuming and prone to oversight, but automated reporting tools help maintain accuracy and compliance.
6. Cybersecurity and Data Protection
With the increasing adoption of digital technologies, cybersecurity is a growing concern in medical device manufacturing. Manufacturers must comply with HIPAA, GDPR, and FDA cybersecurity guidance to protect patient data and prevent cyber threats. Implementing AI-driven automation helps safeguard sensitive information and enforce compliance with data protection regulations.
Addressing these compliance challenges requires workflow automation, which streamlines documentation, enhances quality control, and improves traceability. By integrating automated compliance solutions, medical device manufacturers can navigate complex regulations efficiently while maintaining product integrity and safety.
How Automation Helps Drive Efficiency and Innovation in Medical Device Manufacturing
Medical device manufacturing is a highly regulated and complex industry that requires precision, efficiency, and strict adherence to compliance standards. The increasing demand for faster production, enhanced product quality, and seamless regulatory compliance has made automation an essential tool for manufacturers. By integrating AI-driven automation and robotic process automation (RPA), medical device companies can optimize workflows, improve accuracy, and drive innovation in production processes. Below are some of the key ways automation enhances efficiency and innovation in medical device manufacturing.
1. Improved Compliance Management
Regulatory compliance is a critical aspect of medical device manufacturing, with standards such as FDA’s 21 CFR Part 820, ISO 13485, and EU MDR requiring stringent documentation and approval processes. Automated compliance workflows help standardize these processes by ensuring that all records, approvals, and audit trails are maintained systematically. Automation reduces the risk of human error, improves consistency, and ensures that compliance documentation is always up to date and accessible for audits.
2. Enhanced Quality Control
Maintaining high-quality standards in medical device manufacturing is crucial to ensuring patient safety and regulatory approval. AI-powered automation enhances quality control by detecting defects early in the production cycle. Machine learning algorithms can analyze manufacturing data in real time, identifying inconsistencies, deviations, or errors that could lead to defective products. By automating quality inspections and validation checks, manufacturers can reduce recalls, minimize rework costs, and enhance product reliability.
3. Streamlined Documentation
Traditional documentation methods involve manual record-keeping, which is prone to errors, inefficiencies, and compliance risks. Digital workflow automation ensures that all documentation related to device design, testing, validation, and compliance is stored electronically in a structured and easily retrievable format. Automated documentation management eliminates the need for manual paperwork, enhances traceability, and ensures that documents are updated in real-time. This reduces the administrative burden on teams and allows them to focus on more strategic tasks.
4. Accelerated Production
Manufacturing delays can result in increased costs and delayed time-to-market, affecting competitiveness in the industry. Robotic Process Automation (RPA) optimizes manufacturing workflows by automating repetitive tasks such as material handling, assembly line operations, and product packaging. Automation reduces human intervention, speeds up production processes, and minimizes bottlenecks in the supply chain. As a result, medical device manufacturers can achieve faster production cycles, meet market demand efficiently, and scale operations without compromising quality.
5. Increased Traceability and Audit Readiness
Regulatory agencies require complete traceability of medical devices, from raw material sourcing to final product distribution. Automated tracking systems enable real-time monitoring of production workflows, ensuring full visibility of every step in the manufacturing process. This helps manufacturers maintain compliance with regulations while making audits more efficient and transparent.
6. Facilitating Innovation in Manufacturing Processes
Automation not only enhances efficiency but also drives innovation in medical device manufacturing. AI-driven predictive analytics help manufacturers identify process inefficiencies, optimize resource allocation, and improve production planning. The integration of smart manufacturing techniques, such as IoT-enabled devices and digital twins, allows companies to simulate and refine production workflows before implementation. These innovations lead to reduced waste, optimized production cycles, and improved product development.
By adopting workflow automation, medical device manufacturers can significantly enhance operational efficiency, maintain compliance with stringent regulations, and foster continuous innovation. Automating processes enables businesses to remain competitive, meet evolving market demands, and improve the overall quality of medical devices.
Automation plays a crucial role in overcoming regulatory and operational challenges in medical device production. Key benefits include:
- Improved Compliance Management: Automated workflows ensure adherence to FDA and MDR regulations by standardizing documentation and approval processes.
- Enhanced Quality Control: AI-powered automation identifies defects early in the production cycle, reducing recalls and rework.
- Streamlined Documentation: Digital record-keeping eliminates manual errors and ensures real-time access to compliance documents.
- Accelerated Production: Robotic process automation (RPA) optimizes manufacturing workflows, reducing production delays and improving efficiency.
What is Design for Automation?
Design for Automation (DFA) is a strategic approach that integrates automation principles into the early stages of medical device design. The goal is to develop products that are optimized for automated manufacturing, minimizing manual interventions while maximizing efficiency, accuracy, and scalability. DFA ensures that medical devices can be assembled, tested, and packaged with minimal human involvement, thereby improving overall production speed and reducing costs.
Medical device manufacturers must consider multiple factors when implementing DFA, including material selection, component standardization, assembly techniques, and compliance with industry regulations. By designing medical devices with automation in mind, manufacturers can enhance product quality, streamline production workflows, and meet stringent regulatory requirements more efficiently.
Key aspects of DFA include:
- Material Selection: Choosing materials that are compatible with automated assembly and handling.
- Component Standardization: Designing parts with uniform shapes and sizes to enable seamless integration into automated production lines.
- Modular Design: Creating devices with interchangeable components that simplify assembly and maintenance.
- Automation-Friendly Assembly Techniques: Reducing the need for manual adjustments by designing devices that can be precisely assembled using robotic automation.
- Regulatory Compliance: Ensuring that the device meets FDA, MDR, and ISO 13485 standards right from the design phase.
By incorporating DFA principles early in the development process, medical device manufacturers can achieve greater consistency, improved production scalability, and reduced time-to-market.
How Design for Automation Benefits the Medical Industry
Design for Automation (DFA) provides significant advantages for the medical device industry by improving efficiency, ensuring compliance, and enhancing product quality. By integrating automation principles early in the design phase, manufacturers can optimize production workflows, reduce costs, and meet regulatory standards more effectively. Below are the key benefits of DFA in medical device manufacturing:
Reduced Manufacturing Costs
One of the most significant benefits of DFA is cost reduction. By designing medical devices specifically for automated assembly, manufacturers can minimize labor costs and reduce dependency on manual processes. Automated production lines require fewer human interventions, lowering labor expenses and the likelihood of human errors. Additionally, standardized components and modular designs reduce material waste, further lowering production costs. This streamlined approach ensures cost-efficient mass production without compromising quality.
Enhanced Product Consistency
Automation eliminates variability in manufacturing, ensuring that every medical device meets the same quality and performance standards. DFA focuses on precision engineering, making it easier for machines to assemble components with accuracy and repeatability. This results in fewer defects, improved product reliability, and reduced rework or recalls. By reducing inconsistencies in manufacturing, companies can maintain high-quality standards that are essential for regulatory approval and patient safety.
Faster Time-to-Market
The ability to accelerate production without sacrificing quality is crucial in the medical device industry. DFA optimizes product designs for high-speed automated manufacturing, significantly reducing production cycle times. When devices are designed with automation in mind, manufacturers can expedite regulatory approvals by ensuring compliance from the outset. With faster production and approval processes, companies can introduce innovative medical devices to the market ahead of competitors, meeting urgent healthcare needs more efficiently.
Improved Regulatory Compliance
Medical devices are subject to strict regulations, including FDA (21 CFR Part 820), EU MDR, and ISO 13485 standards. DFA ensures that compliance requirements are integrated into the design phase, reducing the risk of regulatory setbacks. By automating critical processes such as documentation, traceability, and validation testing, manufacturers can create audit-ready records and meet compliance standards effortlessly. DFA also facilitates post-market surveillance, ensuring continuous adherence to regulatory frameworks throughout the product lifecycle.
By adopting DFA principles, medical device manufacturers can achieve greater efficiency, cost savings, and regulatory alignment while maintaining the highest standards of product quality and safety.
End-to-end workflow automation
Build fully-customizable, no code process workflows in a jiffy.
Applications of Workflow Automation in Medical Device Manufacturing
Medical device manufacturers face increasing pressure to maintain compliance, enhance quality control, and streamline operations. Workflow automation plays a crucial role in addressing these challenges by integrating automated systems that enhance accuracy, efficiency, and traceability. The following are key applications of workflow automation in medical device manufacturing:
1. Regulatory Documentation Management
Medical device manufacturers must comply with stringent regulatory requirements, including FDA 21 CFR Part 820, EU MDR, and ISO 13485. Manual documentation processes are time-consuming and prone to human errors, which can lead to compliance issues. Automated documentation workflows ensure that all compliance records, approvals, and audit trails are maintained in a centralized system. This enhances accessibility, minimizes errors, and improves audit preparedness.
2. Supply Chain Optimization
Medical device manufacturing relies on a complex supply chain that includes multiple vendors, raw material suppliers, and logistics partners. AI-powered workflow automation helps manufacturers track inventory levels, coordinate with vendors, and forecast demand more accurately. By automating procurement and inventory management, businesses can prevent stock shortages, optimize costs, and ensure uninterrupted production workflows.
3. Quality Assurance and Testing
Quality control is a critical aspect of medical device manufacturing, as defective products can result in serious safety risks and regulatory violations. Automated quality assurance workflows use AI-driven analysis to identify defects, conduct thorough inspections, and generate real-time compliance reports. Automation ensures that all quality control processes are standardized, reducing the chances of human error and improving overall product reliability.
4. Change Management Compliance
Regulatory agencies require manufacturers to document and validate any changes made to product design, materials, or production processes. Automated change management workflows ensure that all modifications go through a structured approval process. By integrating digital approvals, notifications, and audit trails, businesses can maintain full transparency and compliance with regulatory standards, preventing unauthorized changes from disrupting production.
5. Risk Management and Traceability
Regulatory compliance mandates complete traceability of medical devices from raw material sourcing to distribution. Automated risk management workflows provide a detailed audit trail, allowing manufacturers to track every stage of production. This improves response times during recalls, enhances product safety, and ensures that all regulatory reporting requirements are met efficiently.
By implementing workflow automation, medical device manufacturers can improve operational efficiency, ensure compliance, and maintain high product quality standards while reducing manual interventions and production delays.
Automating Medical Device Manufacturing Workflows with Cflow
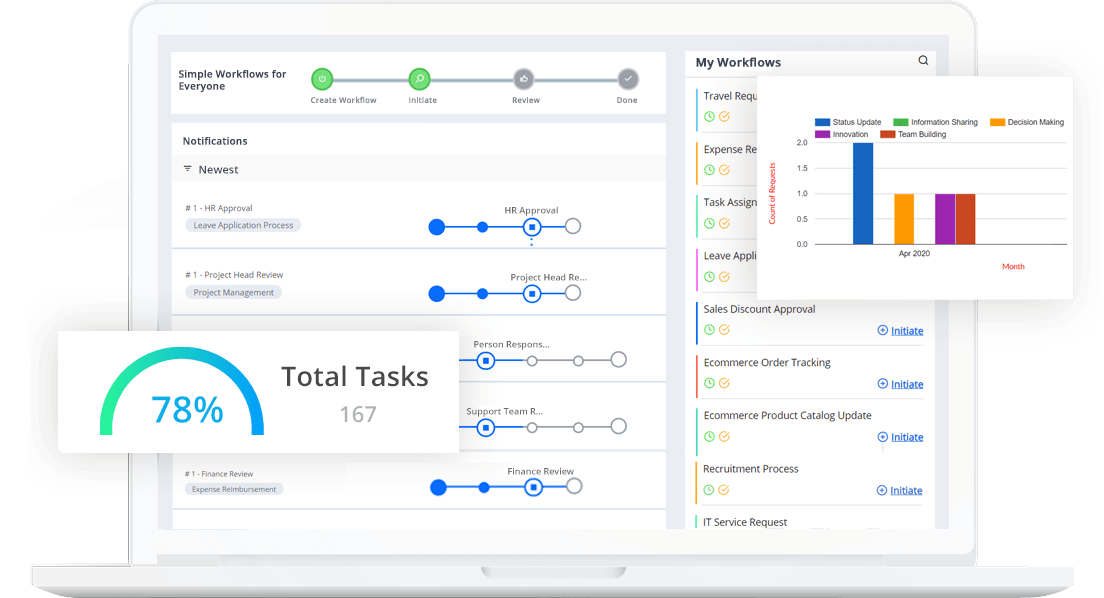
Cflow is a leading workflow automation platform designed to help medical device manufacturers optimize compliance and operational efficiency. Key features of Cflow include:
- Automated Compliance Workflows: Streamlines FDA and MDR documentation requirements, ensuring regulatory adherence.
- Quality Control Automation: Enhances defect detection and ensures standardized quality checks.
- Real-Time Monitoring and Reporting: Provides real-time insights into manufacturing processes and compliance status.
- Integration with ERP and Quality Management Systems (QMS): Seamlessly connects with existing enterprise solutions for smooth workflow execution.
- Secure Cloud-Based Storage: Ensures safe and compliant storage of medical device records.
Conclusion
Medical device manufacturing is a highly regulated industry that requires precision, compliance, and efficiency. Workflow automation is revolutionizing the sector by streamlining documentation, improving quality control, and ensuring compliance with FDA and MDR regulations. By integrating automation solutions like Cflow, manufacturers can eliminate inefficiencies, enhance traceability, and drive innovation in medical device production.
Start optimizing your medical device manufacturing workflows with Cflow today!
FAQs
- Why is compliance important in medical device manufacturing?
Compliance ensures that medical devices meet safety, quality, and regulatory requirements, preventing legal issues and product recalls. - How does automation improve medical device manufacturing?
Automation enhances efficiency, reduces errors, streamlines documentation, and ensures compliance with FDA and MDR regulations. - What is Design for Automation (DFA)?
DFA is an approach that designs medical devices for compatibility with automated manufacturing, reducing costs and improving production efficiency. - How does workflow automation help with compliance?
Workflow automation standardizes regulatory processes, maintains accurate documentation, and ensures timely audits and approvals. - Can workflow automation integrate with existing manufacturing systems?
Yes, platforms like Cflow integrate seamlessly with ERP and Quality Management Systems (QMS) to optimize manufacturing workflows. - What role does AI play in medical device manufacturing?
AI enhances defect detection, optimizes supply chain management, and improves regulatory compliance through predictive analytics and automation.
What should you do next?
Thanks for reading till the end. Here are 3 ways we can help you automate your business:

Do better workflow automation with Cflow
Create workflows with multiple steps, parallel reviewals. auto approvals, public forms, etc. to save time and cost.

Talk to a workflow expert
Get a 30-min. free consultation with our Workflow expert to optimize your daily tasks.

Get smarter with our workflow resources
Explore our workflow automation blogs, ebooks, and other resources to master workflow automation.
What would you like to do next?
Automate your workflows with our Cflow experts.